Blood pressure plays a crucial role in maintaining healthy circulation and skin integrity, but many people don’t realize that poor circulation, dry skin, and cracked heels can increase the risk of serious skin infections like cellulitis. During dry weather or in people with chronic conditions, the skin barrier weakens, creating small openings for bacteria to enter. When combined with circulation issues linked to uncontrolled blood pressure, the body’s ability to fight infection reduces, increasing the chances of cellulitis.
This blog explains the connection between dry and cracked skin, blood pressure, and cellulitis—along with practical steps to prevent complications.
What Is Cellulitis?
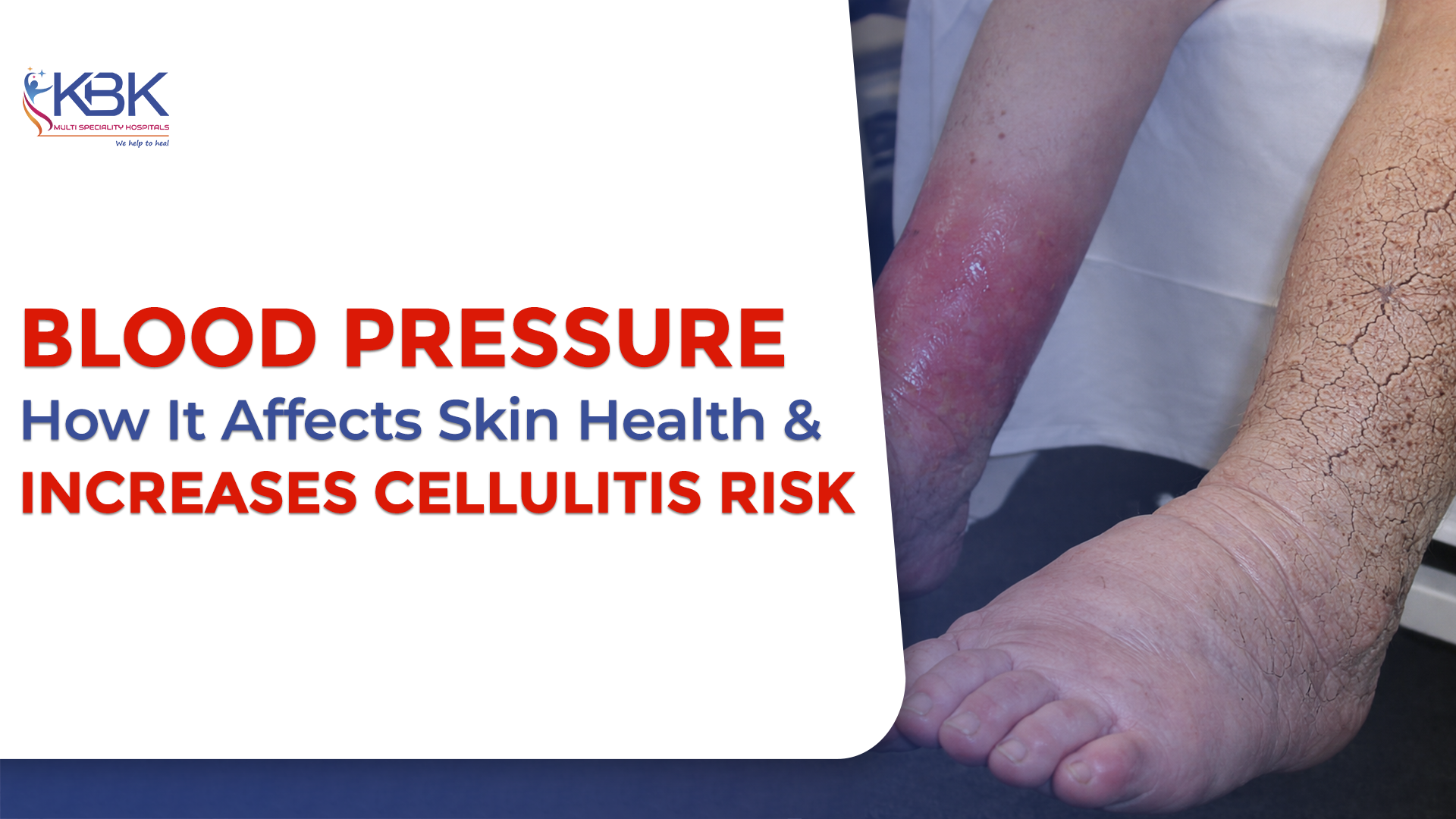
Cellulitis is a bacterial infection of the deeper layers of the skin and soft tissues. It usually starts when bacteria enter through tiny breaks in the skin—such as dry cracks, cuts, or fissures on the feet and legs.
From clinical experience, doctors often see cellulitis develop in patients who have:
- Dry, cracked skin on feet or legs
- Swelling in the lower limbs
- Circulation problems related to blood pressure issues
- Diabetes or nerve damage
These small skin openings may look harmless, but they can become entry points for infection.
How Blood Pressure Affects Skin Health
Blood pressure directly affects blood flow to the skin. When blood pressure is poorly controlled or circulation is compromised, the skin receives less oxygen and fewer nutrients. This can lead to:
- Dryness and rough skin texture
- Delayed skin repair
- Weakened skin barrier
- Slower healing of small cracks and wounds
Over time, reduced circulation linked to blood pressure problems makes the skin more vulnerable to infections like cellulitis.
Why Dry and Cracked Skin Increases Cellulitis Risk
Dry and cracked skin creates microscopic breaks that allow bacteria to enter the body. In real-world medical settings, many cellulitis cases begin with:
- Cracked heels
- Dry patches between toes
- Small fissures caused by dryness
- Minor cuts that fail to heal
When blood pressure and circulation are not optimal, the immune response in the affected area is weaker. This combination significantly increases the risk of cellulitis developing and spreading.
Who Is at Higher Risk?
People with the following conditions should be especially careful about dry skin and blood pressure management:
| High or uncontrolled blood pressure | Diabetes | Poor blood circulation in legs |
| Varicose veins or leg swelling | Elderly individuals | Those with a history of cellulitis |
These groups are more likely to develop skin cracks and are at higher risk of infections.
Early Signs of Cellulitis You Should Not Ignore
Watch for these early symptoms, especially if you have dry skin and blood pressure issues:
- Redness that spreads
- Swelling and warmth in the skin
- Pain or tenderness
- Fever or chills
- Skin that looks shiny or tight
Early medical attention can prevent complications and hospitalization.
How to Prevent Cellulitis When You Have Dry Skin and Blood Pressure Issues
Here are practical, doctor-recommended prevention steps:
1. Maintain Healthy Blood Pressure
Keeping blood pressure under control improves circulation, which helps the skin heal faster and fight infections.
2. Moisturize Daily
Use fragrance-free moisturizers to prevent cracks, especially on feet and legs.
3. Inspect Your Skin Regularly
Check for small cuts, cracks, or redness—especially if you have circulation problems.
4. Protect the Skin Barrier
Avoid walking barefoot, and use protective footwear to prevent injuries.
5. Treat Minor Wounds Early
Even small cuts should be cleaned and covered properly to avoid bacterial entry.
When to See a Doctor
If redness spreads quickly, swelling increases, or pain worsens—seek medical care immediately. People with blood pressure problems or poor circulation should not delay treatment, as cellulitis can progress rapidly without timely care.
Why Early Care Matters
Untreated cellulitis can lead to serious complications, including abscess formation, tissue damage, and in severe cases, bloodstream infections. Managing blood pressure, keeping skin healthy, and acting early can prevent long-term problems and improve recovery outcomes.
Conclusion
Blood pressure management and proper skin care go hand in hand when it comes to preventing cellulitis. Dry and cracked skin may look minor, but when circulation is affected, these small breaks become serious risk factors for infection. By maintaining healthy blood pressure, protecting the skin barrier, and seeking early medical care, you can significantly reduce the risk of cellulitis and its complications.