Gangrene feet are a serious medical condition that often begin with what seems like a minor foot problem—such as a small cut, blister, ingrown nail, or ulcer. When infections are ignored or circulation is poor, bacteria can spread into deeper tissues, cutting off blood supply and causing tissue death. In real clinical practice, delayed medical attention is one of the biggest reasons foot infections progress into gangrene. Understanding how this happens, who is at risk, and what early signs to watch for can help prevent severe complications, including amputation.
What Is Gangrene in the Feet?
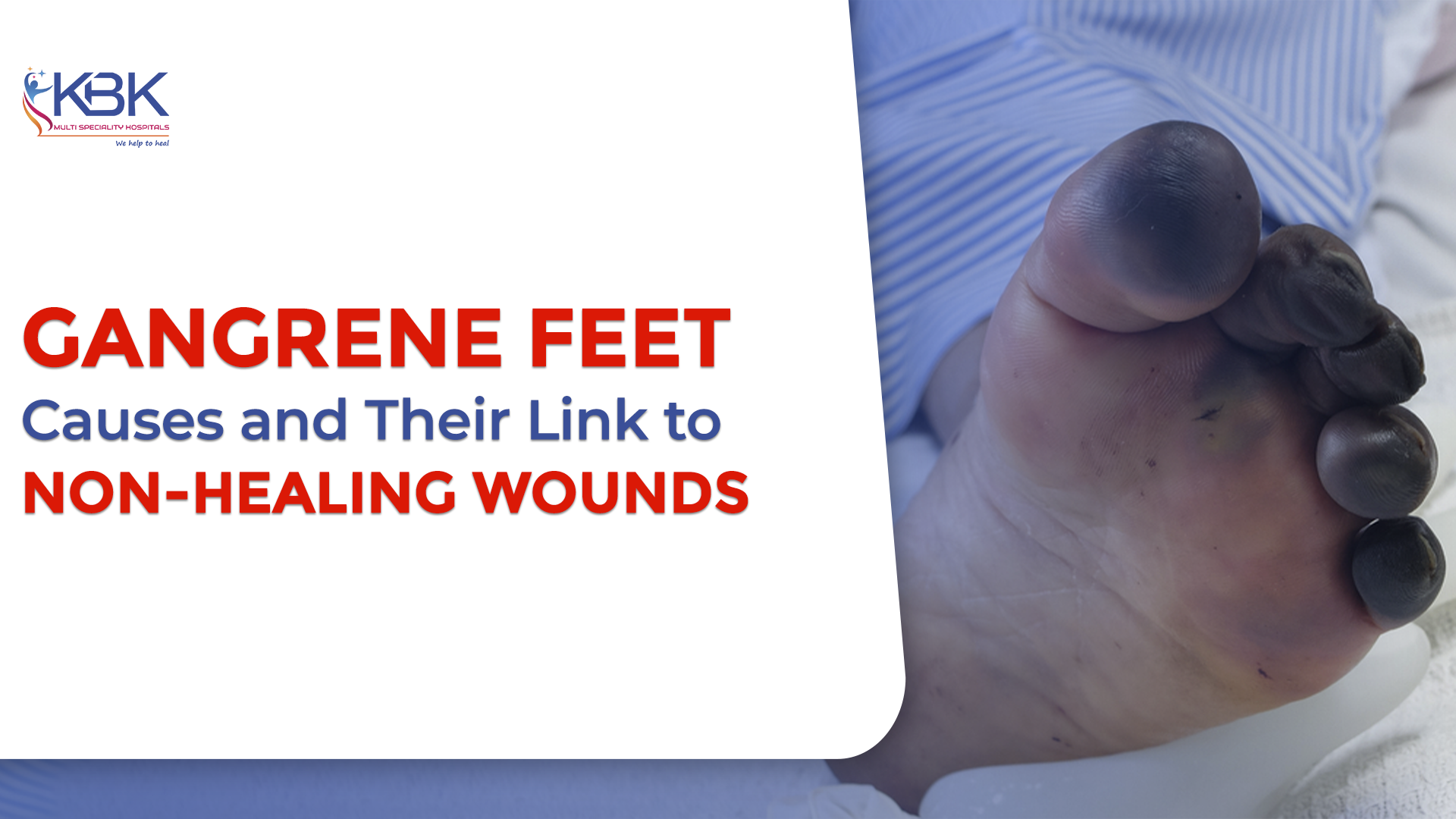
Gangrene refers to the death of body tissue due to a lack of blood flow, severe infection, or a combination of both. When it affects the feet, it is usually associated with vascular disease, diabetes-related nerve damage, and chronic wounds. Doctors commonly classify gangrene into types such as dry gangrene (caused mainly by poor circulation), wet gangrene (caused by infection), and gas gangrene (a rare but life-threatening infection). Each type can affect the feet, but wet gangrene is most often linked to untreated infections.
How Infections Progress into Gangrene
In many patient cases, gangrene feet start with a wound that fails to heal. Bacteria enter through broken skin and cause infection. As swelling and inflammation increase, small blood vessels become compressed or blocked, reducing oxygen supply to the tissue. Without adequate blood flow, the body’s immune response weakens, allowing the infection to spread further. Over time, the affected tissue begins to die, leading to discoloration, foul odor, and severe damage.
People with reduced sensation in the feet, such as those with diabetic neuropathy, may not feel pain early on. This delay in noticing symptoms allows infections to worsen silently until the condition becomes advanced.
Early Signs and Symptoms to Watch For
Early recognition is critical in preventing gangrene feet from worsening. Warning signs include:
- Persistent or worsening pain, or loss of sensation
- Redness, swelling, and warmth around a wound
- Skin color changes to blue, purple, brown, or black
- Foul-smelling discharge from wounds
- Non-healing ulcers or blisters
- Fever or signs of systemic infection
Medical experts emphasize that any rapidly worsening foot infection should be treated as an emergency.
Who Is Most at Risk?
Individuals at higher risk of developing gangrene feet include:
- People with diabetes
- Those with poor blood circulation or peripheral arterial disease
- Smokers
- Older adults
- Patients with weakened immune systems
- People with a history of foot ulcers or previous infections
These groups require regular foot examinations and early medical intervention for even minor wounds.
Diagnosis and Treatment Options
Doctors diagnose gangrene through clinical examination, imaging, blood tests, and sometimes vascular studies to assess blood flow. Treatment focuses on removing infected tissue, controlling infection with appropriate medications, restoring blood flow where possible, and providing advanced wound care. In early stages, limb-saving procedures may prevent further tissue loss. In advanced cases, surgical intervention may be necessary to stop the spread of infection.
Prevention: Protecting Your Feet
Preventing gangrene feet involves daily foot inspection, proper hygiene, moisturizing to avoid cracks, wearing protective footwear, and treating wounds early. Managing chronic conditions such as diabetes and circulation problems is equally important. Patients who attend regular medical check-ups and seek care at the first sign of infection have significantly better outcomes.
Conclusion
Gangrene feet often result from untreated infections combined with poor blood flow and delayed care. Early detection, prompt medical treatment, and consistent foot care are key to preventing serious complications. With timely intervention, many patients can avoid severe tissue damage and protect their mobility and quality of life.